The rotator cuff is a sheath of muscles which surrounds the shoulder joint, it helps to stabilise the shoulder and powers the wide range of movements which allow positioning of the hand. The rotator cuff may be affected by degenerative disease and injury leading to the development of pain, limitation of movements, difficulty with everyday tasks such as reaching or dressing and disturbance of sleep. Initial management includes rest, tablets, physiotherapy and steroid injection which may give only temporary relief. Apart from standard evaluation with plain x-ray you may have undergone more detailed imaging in the form of ultrasound or MRI scan which may pick up a tear in the rotator cuff.
Close by at the outer end of the collar bone is the acromioclavicular joint which may be affected by arthritis and which may also be a source of symptoms.
Arthroscopy, in other words the keyhole examination of the shoulder, is the first step and is used to identify the extent of disease or injury before a decision is made on what form surgery should take. The rotator cuff tendons are inspected from within the shoulder joint and also externally in the subacromial space or bursa which lies just under the bone at the apex of the shoulder. Impingement may be identified where the worn or frayed rotator cuff tendons are catching under the acromion. Alternatively a worn tendon may have progressed to a torn tendon sometimes as a result of injury and if so a defect or tear will be identified. Other structures which may contribute to symptoms are checked including the long tendon of biceps which runs through the shoulder joint, the joint surfaces which may be affected by arthritis and the structures around the edge of the socket (labrum and capsule) which may be damaged as the result of dislocation.
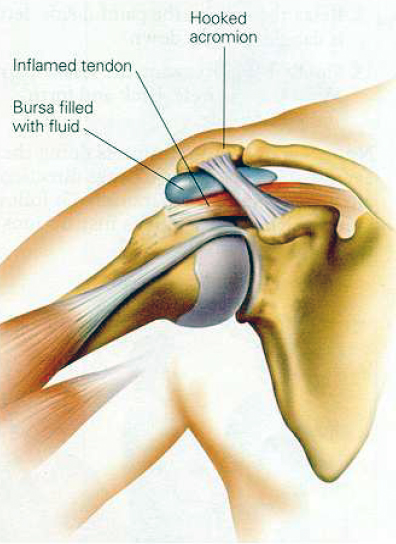
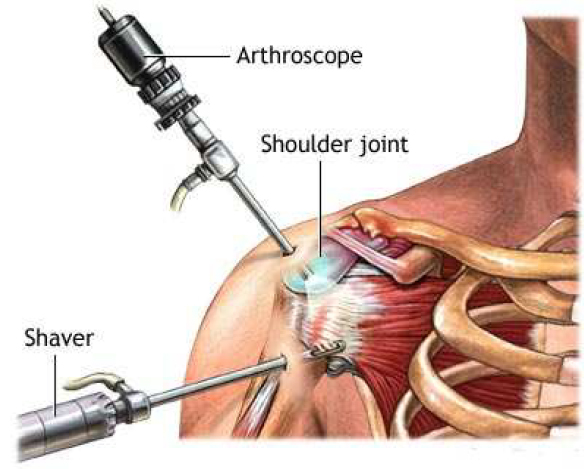
Once the surgeon has compiled all the above information a decision can be made as to what treatment would be suitable and most likely to succeed. For example, if a massive defect is found in the rotator cuff the decision may be that repair is not possible and that treatment will be confined to trimming of soft tissues and bone purely as a pain relieving measure. If the diagnosis is of subacromial impingement without a tear then arthroscopic acromioplasty is performed which entails the trimming of ligament and bone from the undersurface of the acromion at its front edge.
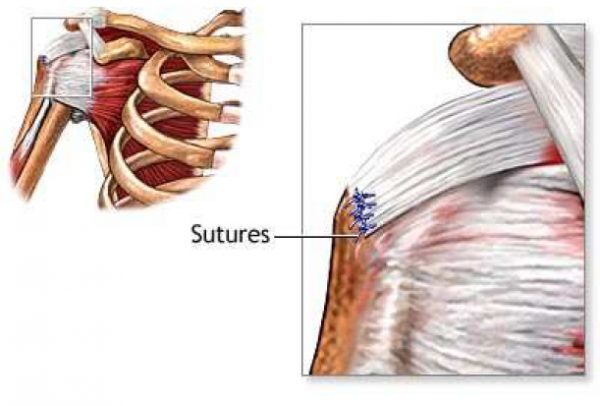
If a cuff tear is identified then assuming it is repairable reattachment of tendon to bone at the top end of the humerus is performed by open operation or more commonly nowadays by a keyhole technique using suture anchors, this decision depends upon the complexity and size of the tear and also upon the experience and training of the surgeon.
Other procedures which may be necessary include tenotomy (division) or tenodesis (fixation) of the long tendon of biceps and excision (trimming) of the outer end of the clavicle for arthritis in the acromioclavicular (AC) joint. Depending on the findings at arthroscopy more than one procedure may be necessary.

In general for any operation other than cuff repair early movement is encouraged as pain permits. Outpatient physiotherapy may be necessary, however you should expect to perform the exercise regime regularly and by yourself.
If you have undergone a cuff repair then a shoulder immobiliser sling will be applied for six weeks during which period you will be limited to pendulum exercises and passive movements, in other words lifting of the operated limb by the physiotherapist or by yourself using the other hand. This is designed to minimise stiffness and at the same time to protect the stitches in the rotator cuff. After the initial six week period the sling is discarded and active movement progresses again under the supervision of the physiotherapists. The key principle to remember is that recovery from this type of surgery takes a minimum of three months and if cuff repair is necessary at least double that. Even if there is no early benefit it is well worth persevering with your rehabilitation as your shoulder may potentially improve up to a year from surgery. Overall the anticipated success rate is around 80%.
Before your admission you should have attended the preassessment clinic in order to check your general fitness for anaesthesia and also to meet your surgeon or the surgical assistant in order to sign a consent form. This visit gives an ideal opportunity to clarify any queries or doubts on your part, it also gives the surgical team the chance to check that surgery remains appropriate and that you are having the correct operation. If you are coming into hospital on the day of your surgery it is important you do not eat for six hours or drink for two hours prior to your admission to hospital. (Only drink black tea, black coffee or water). Bring loose comfortable clothing into hospital without awkward or numerous fastenings On admission you will be examined by an anaesthetist who will assess your fitness for surgery and discuss the type of anaesthetic including regional block which may render your arm numb for about 12 hours after surgery. A pre-medication drug may be prescribed before your operation to help you relax. You will be asked to wear a theatre cap and gown and a nurse and porter will escort you to theatre.
- An oxygen mask on your face, this is removed on the anaesthetist’s instructions
- Temporary numbness and weakness of the arm if you have had regional block
- A degree of pain. There will be pain relief prescribed, please ask the nurse if you require it so that you can be kept as comfortable as possible.
- A large bulky dressing on your shoulder for support
- A broad arm sling or antirotation sling, depending on the procedure carried out
You must be fully recovered from the anaesthetic to go home on the same day. However, rotator cuff repair may require an overnight stay in hospital. This allows the nurses to change your dressing as it normally becomes very wet.
Before discharge your dressing will be reduced. Dressings may be removed at 48 hours from surgery, assuming the wounds are healthy. You can then take a shower. Sutures if absorbable will need to be trimmed and if nonabsorbable will need to be removed at one week, this can usually be done by your general practitioner.
You may continue to experience discomfort or pain for some weeks after the procedure. You will be advised to take mild painkillers prior to discharge.
Arrangements for outpatient physiotherapy will be made if necessary. Following cuff repair outpatient physiotherapy is mandatory and should commence within a few days, if this does not take place then please contact the Matrix Office or the consultant’s personal assistant immediately.
After an arthroscopic procedure without cuff repair driving is usually possible at three weeks and non-manual duties below shoulder level at six weeks. Following cuff repair you will not be able to drive for at least eight weeks, that is two weeks after coming out of the sling, light manual work below shoulder level should be manageable by three months from operation.
A follow up appointment will be made for you to see the surgeon, timing depends upon the nature of surgery. Following cuff repair the first appointment is usually at six weeks, after other arthroscopic procedures it is normally at three months.